Long-term Strategy
Long-term Strategy

MUCH-NEEDED CARE An aging population and growing resident acuity means more investments in long-term care are needed so that nurses like Daniela Smitlener can provide seniors with the care they need.
There's a demographic shift taking place across the country, and as the population continues to age, there are growing calls for governments to acknowledge the increasing demands on long-term care facilities and other areas of the health-care system that are feeling the pressure.
Canada's population is rapidly aging – a trend that will continue for the next couple of decades. Our senior population – those aged 65 or older – is expected to climb to 10 million by 2037, an increase of 68 percent.
This demographic shift is being felt in BC, where projections indicate that by 2031 one-in-four people will be over 65. This is nearly five percent higher than the Canadian average. Questions are already being raised about what this will mean for health care in the province, and for the nurses who play a vital role in promoting the health and well-being of seniors every day.
The BC Nurses' Union is stepping up efforts to raise awareness among policy makers and the public about the importance of investing in senior's care now and into the future. The challenging conditions in most of the province's long-term care facilities are just one indication of the need to do more to ensure that seniors get the care they need.
"We are concerned about the lack of attention this demographic often receives."
Currently, the majority of long-term care facilities aren't anywhere close to meeting patient care targets set out by the provincial government. And nurses are saying it's increasingly difficult to provide safe patient care.
"We know that most facilities around the province are unable to provide the daily average of 3.36 hours of direct care per resident, set as a goal by the provincial government," says BCNU President Christine Sorensen. "While our nurses take pride in playing a vital role in promoting the health and well-being of seniors, the erosion of health support services is making it increasingly difficult to succeed."
For nurses working in BC's long-term care sector, it's a hard reality that constantly tests their ability to provide quality resident care. Chronic underfunding, short staffing and heavy workloads plague an already overrun system, and that's taking a toll on BCNU members who work in the sector. Recruitment and retention challenges continue to exist everywhere, especially in smaller, rural communities around the province.
Patient acuity has also shifted, and seniors' health care needs are becoming more complex. For example, nine seniors are diagnosed with dementia every hour in Canada. And in 2015 there were over 61,000 people in BC living with dementia.
TAKING COORDINATED ACTION
BCNU's commitment to seniors and long-term care nurses comes in many different forms. The union has developed a senior's strategy working group consisting of elected members and researchers. The group meets monthly to discuss priorities and strategies on how to best shine a light on the needs in long-term care.
BCNU's regional chairs marked National Seniors Day on Oct. 1 by visiting long-term care facilities in every union region in the province, dropping off chocolates and thanking long-term care members for the valuable work they do every day.
And on a national level, BCNU is one of many organizations, including the Canadian Federation of Nurses Unions and the Canadian Nurses Association, that are calling for a national seniors strategy that would see the federal government play a central role to help address seniors' health-care needs across the continuum of care (see sidebar: long-term care just one part of the solution).
"A national seniors strategy demands a coordinated set of federal, provincial and municipal policies and programs that appropriately address the needs and concerns of seniors across the country," says Sorensen. "We are concerned about the lack of attention this demographic often receives by the government. The statistics all point in the same direction – we need a plan in place to ensure BC's and the rest of the country's rapidly aging population will be taken care of."
Investing in seniors' care is also one of BCNU's top priorities in the federal election. Work is underway to create dialogue with all current and prospective MPs on how they plan to improve care and support for seniors. "Our long-term care nurses are already under pressure to provide care under unrealistic expectations," says Sorensen. "How will the candidates from every party seeking to form the new federal government work with the provinces and communities to manage these needs over the next decade?"
Sorensen notes that improving seniors' care also means supporting integrated primary and community care networks that provide care closer to home. BCNU is currently working with health employers to ensure that nurses play a central role in shaping these networks and providing the practice supports that are needed to elevate standards of care.
"This is something BCNU will continue to advocate for," says Sorensen. "Effective primary and community care networks allow for people to live at home longer, and they take the pressure off emergency departments and long-term care facilities. In order to take care of our aging population, decision makers will have to work closer with health providers to ensure we are all working towards the same goal – provide the best care for our seniors. It's what they deserve." •
UPDATE (October 2019)
WAITING FOR LONG-TERM CARE IN BC
BC’s Office of the Seniors Advocate annual Monitoring Seniors Services reports provide a running snapshot of the status of seniors’ services in BC – including long-term care. The following numbers are taken from the office’s most recent report published in Dec. 2018.
On March 31, 2018, the number of people on the waitlist increased 7% over the previous year to 1,379; 1,039 were waiting in the community and 340 were waiting for transfer from a hospital.
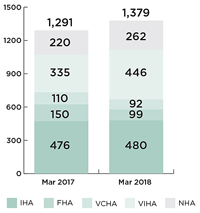
The average wait time for people on the waitlist on March 31, 2018 was 138 days ranging between 41 days in Fraser Health and 282 days in Northern Health.
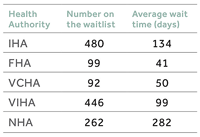
Source: Monitoring Seniors Services 2018. Office of the Seniors Advocate
NATIONAL SENIORS STRATEGY
Long-term care just one part of the solution
When it comes to addressing seniors’ health, the key issues and areas of concern vary across the continuum of care and differ from province to province. That’s why the call for an effective national seniors strategy contains proposals that focus on care throughout the health-care system – with national standards for long-term care being just one part of the solution.
SOCIAL DETERMINANTS OF HEALTH
Efforts to improve wellness and prevention must go beyond the health-care system to encompass the life factors that shape each person’s overall health and well-being. Income security, safe housing and access to good food and social connections are all issues to be addressed by a national seniors strategy.
PRIMARY CARE
An effective primary care system is crucial for keeping seniors out of hospitals. Primary care providers can manage the complex needs of seniors better when integrated with specialist care and given greater training in geriatrics and palliative care. Stronger links between providers and the community services their patients need would also help.
HOME CARE AND COMMUNITY SUPPORT
Looking after seniors at home is cost-effective and what most people want. But care and funding home support vary greatly across Canada, and most care is provided by unpaid family and friends. A national seniors strategy should offer families more support such as tax breaks, leave and respite.
ACUTE AND SPECIALTY CARE
Acute-care hospital stays are often preceded by long waits for specialists and treatment. After, poor coordination between the acute and community sectors often traps seniors in hospital, awaiting a long-term care bed or home care. These poor transitions between levels of care are known to put patients at risk. A national seniors strategy must emphasize better coordination of care.
LONG-TERM CARE
Most residents of long-term care are over 85 and frail. Many have considerable cognitive and health challenges. As Canadians live longer, demand for long-term care increases, but older care homes are not designed for today’s high-need patients. Long-term care is also expensive. A national seniors strategy should include national standards of care and a plan for funding it.
PALLIATIVE CARE
Demand for end-of-life care that focuses on quality of life and death, rather than treatment, is increasingly in demand, but access to it is limited and poorly coordinated. A team approach and more training for health-care providers, supported by national standards, would increase availability.