The Deadliest Year
The Deadliest Year
Rising numbers of preventable deaths in 2020 means more action is needed to confront the province's worst public heath emergency
Tommy was helping a friend break up some cement and he popped a disk," Deb Picco recalls.
After the back surgery that followed the injury, her son was prescribed Oxycontin to manage the pain. "But the pain never left. He ended up having two more surgeries and he was in constant pain despite the drugs that he was taking," says Picco.
"That's what the original problem was, and then he gradually got into heavier and heavier drugs."
Unfortunately, the treatment options available to Tommy were not enough.
"He'd been through rehab a couple of times and detox a couple times," says Picco. "There were lots of changes in him that you would see on account of the drug use, you know, but they were not able to do anything to help that pain."
Tommy was 36 when he died from opioid poisoning last October. It was the end of a journey with substance use that began when he was a 21-year-old young man.
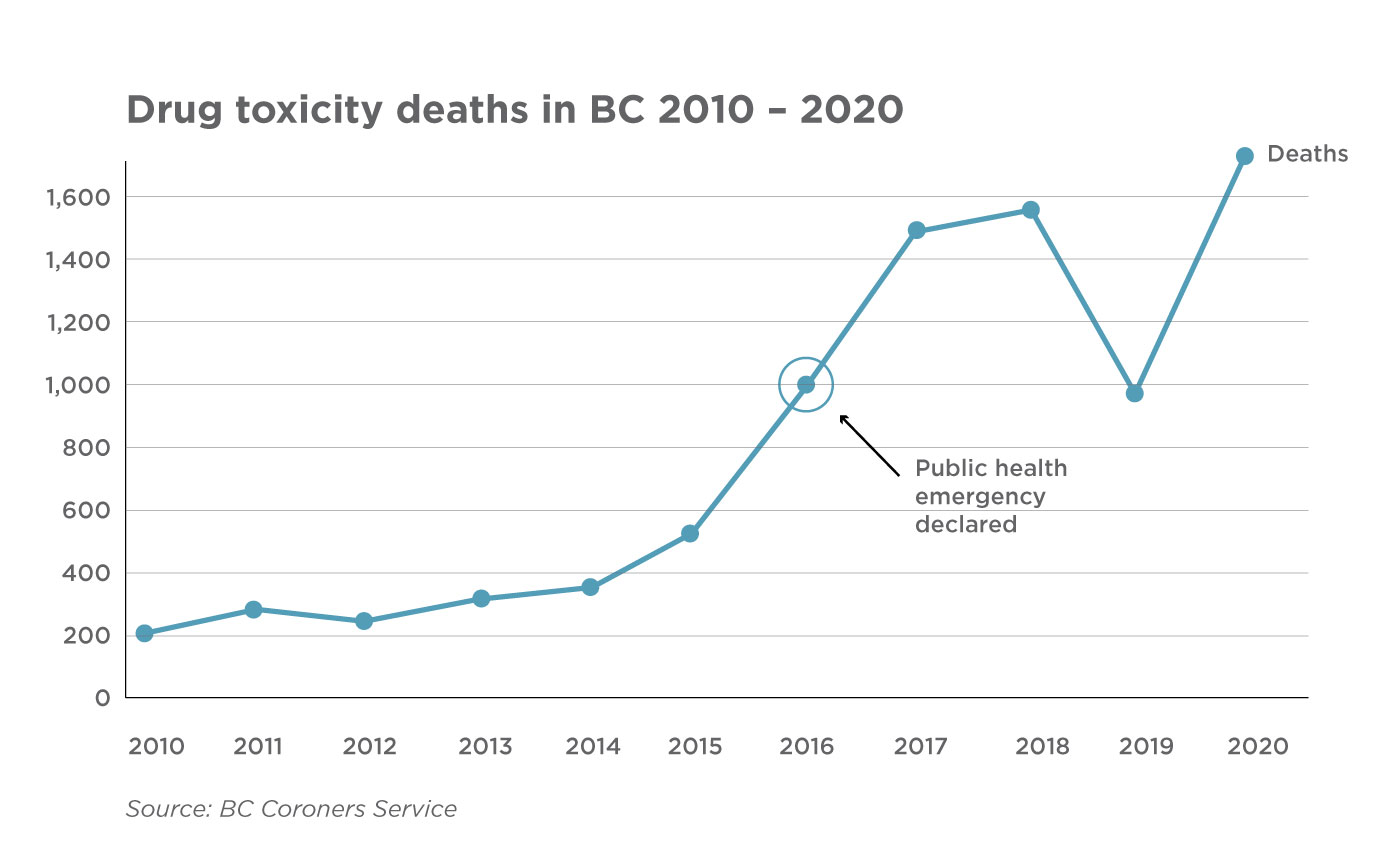
His death came almost five years after the province's overdose crisis was first declared a public health emergency in 2016, after fentanyl began entering the drug supply three years earlier.
Sadly, BC continues to endure a terrible burden of death on account of the toxic drug supply. And since 2016, the number of people who have died from drug toxicity in BC has risen tragically and dramatically.
According to BCs chief coroner Lisa Lapointe, at least 1,716 British Columbians lost their lives in 2020 without access to a regulated, safe alternative to poisoned illegal drugs. This represents the most deaths ever in a single year in this province due to an unnatural cause, and an alarming death rate of 33.4 per 1,000 people – about five deaths per day on average.
The 1,716 number surpasses the 1,549 people who died in 2018, up until now the deadliest year, and is a 74-percent increase from last year's 984 deaths.
As has been the pattern throughout this public health emergency, the vast majority of those dying are inside a private residence.
Fentanyl continues to drive the health crisis. The substance was found in over 86 percent of deaths between 2017 and 2020.
According to Lapointe, the toxic drug market remains the number one public health risk in BC, with deaths due to toxicity surpassing the number of deaths due to suicide, motor vehicle collisions, homicide and prescription drug deaths combined.
"People are dying in communities across BC and from all walks of life. They leave behind broken hearted families, friends and co-workers," she said during an April news conference to mark the five-year anniversary of the crisis.
Sadly, she also reported that in 2020 the emergency had become far worse, and there is seemingly no end in sight.
Lapointe said there is no question that harm reduction measures introduced since the public health emergency was declared have had a measurable effect of reducing deaths in 2019. The widespread provision of naloxone, the opening of overdose prevention sites and supervised consumption sites and drug checking services reduced poisonings and the number of deaths decreased in our province.
However, since the start of the COVID-19 pandemic, drug toxicity deaths have again been increasing at an alarming and steady rate. "With the pandemic, access to harm reduction measures was reduced, people self-isolated and the harms associated with the illicit drug market returned with a vengeance," said Lapointe.
A Renewed Call for Action
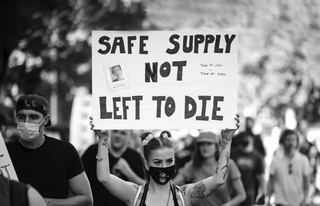
The five-year anniversary of the health emergency, along with the spike in opioid deaths, has prompted renewed calls for action to address the crisis.
BCNU is one of those organizations that's joining with advocates in calling for increased investments in harm reduction services like safe consumption sites, better access to safe supply such as prescribed pharmaceutical alternatives, province-wide investments in mental health, treatment and recovery services, and ending the criminalization of people who use drugs.
"BC's nurses see the effects of the toxic drug supply every day, including during the COVID-19 pandemic," says BCNU President Christine Sorensen. "They continue to work tirelessly to provide care while this province manages two public health emergencies. It's time the government provides more effective solutions to address this epidemic."
BCNU, along with advocacy group Moms Stop the Harm, which is a network of families impacted by substance-use related harms and deaths, is calling for more action from all levels of government to address the crisis, and for an end to the failed "war on drugs" approach to substance use through the promotion of evidence-based policy change.
Moms Stop the Harm has over 2,000 members, with 1,000 in BC. Most are mothers who have lost children to drug harms. Picco become involved with the group last year, after Tommy's death.
A long-time BCNU activist, Picco retired in 2019. She worked in home care in Maple Ridge, and served on the union's council from 2011 to 2016, as BCNU Simon Fraser region council member.
A STEP BACKWARD
COVID-19 pandemic public health measures have been followed by a spike in the number of overdose emergencies in the province. The numbers are a tragic reversal of the progress that's been made in recent years to reduce the rate of opioid poisoning.
"I heard about Moms Stop the Harm on the news one day when [group spokesperson] Leslie McCain was talking and I found their Facebook page," she says. "Right now I use the group for support. It's for parents or loved ones of people who have died, or people who use substances themselves, who can find other people who know what they're going through."
She says the help she's received from other families who have suffered loss has been invaluable.
"You don't know what it's like until that happens to you. You can imagine it, but it's never quite the same," she explains. "So I'll go on there if I'm having certain feelings or something, and other people go on and just support you, and say 'this is what it was like for me.'"
Still grieving, Picco plans to turn her experience into activism in the future. "My intent is to eventually get into more advocacy work for Moms Stop the Harm."
Like many people who have been affected by the opioid crisis, Picco believes the COVID-19 pandemic has shown what's possible when there is political will.
"The response to COVID-19 tells us that the government is not taking the drug toxicity public health emergency seriously enough. They can put money and resources into pandemic emergencies and choose to ignore other emergencies."
Picco believes that the stigma surrounding substance use is a major factor behind governments' uneven approach to both public health crises, and urges everyone, including nurses, to resist falling prey to many of the stereotypes surrounding substance use.
"It's important to treat people who use substances with an awareness that it is a mental health issue," she says. "I think most of us see people who use substances as a nuisance, as people who are choosing to be like they are."
Picco knows this is not true.
"Just a couple months before Tommy died, he shared how hopeless he felt after struggling with pain for 15 years, seeing no end to it, and realizing he would never work again, be productive or have a family of his own. He had tried but couldn't get away from the substance use and homelessness, and his sense of failing himself and his family."
A growing body of addiction research is showing that people who use substances have often suffered a traumatic experience. "Usually in their childhood or in their youth," says Picco. "We don't always know, but we have to understand that there is usually a cause for their substance abuse."
From Decriminalization of Use to Safe Supply
The decriminalization of people who use drugs is an important step toward removing the stigma surrounding substance use. There is now wide consensus that addiction and substance use is a health-care issue, not a criminal or a moral one, and it should not be addressed by criminalizing personal possession and consumption.
"The current war on drugs has been costly and grossly ineffective and has resulted in widespread stigma toward addiction and against those who use illegal drugs," says Sorensen. "We need to stop treating the most vulnerable members of our society like criminals."
Portugal decriminalized the use of all drugs, including heroin and cocaine, in 2001 and began a major public health campaign to tackle addiction. Sorensen notes that the crisis in that country soon stabilized and in the ensuing years it saw dramatic drops in problematic drug use, infection rates, overdose deaths and drug-related crime. Portugal's mortality rate is now four times lower than the European average.
"We've learned from countries like Portugal that when you decriminalize, people feel safe enough to ask for treatment."
BCNU has also endorsed the Office of the Provincial Health Officer's 2018 special report that provides an analysis of the harms associated with criminal justice-based approaches to drug policy. The report, entitled Stopping the Harm, provides options for amending the province's Police Act in a manner that would guide law enforcement in its interaction with people who use controlled substances. This could include developing a new regulation that would prevent police officers from expending resources on the enforcement of simple possession offences under federal law.
"We just need to ensure that they can be safe in what they are doing."
While possession itself remains illegal, this approach creates alternative pathways for law enforcement to link people to supports and services they may need.
Regrettably, the provincial government dismissed the report's recommendations, claiming the province has no jurisdiction to act because possession of illegal substances is governed by federal law, and that it can't direct police on how to conduct operations.
Legal advocates have since countered this claim, and have argued that enacting legislation to amend the Police Act is within the authority of the province, which bears responsibility for ensuring the health of British Columbians.
Fortunately, de facto decriminalization is already occurring in many areas of BC through the discretion of law enforcement when they interact with people who use drugs.
Last July, the Canadian Association of Chiefs of Police recognized that substance use disorder should be a health priority and not a criminal justice matter, and announced its support for the decriminalization of small amounts of illegal drugs for personal use. This position was also fully endorsed by the BC Association of Chiefs of Police.
And last year the public prosecution service of Canada developed new charging guidelines for simple possession of illegal drugs, only accepting charges where there are extenuating circumstance impacting public safety.
Public health advocates say that treatment and harm reduction measures must be accompanied by improved access to safe opioids.
Despite the progress that's been made to reduce stigma, public health advocates point to the fact that the real danger of a poisoned drug supply remains as long as the production and distribution of non-pharmaceutical opioids and other substances remain illegal.
That's why access to a safe and regulated drug supply is so critical. It's also why BCNU welcomed last September's public health order that authorizes RNs and RPNs to prescribe pharmaceutical alternatives to toxic drugs as a step in the right direction.
"Expanding nurses' scope of practice is one part of the solution to addressing the opioid crisis, especially as deaths continue to climb," said Sorensen when the order was announced. "However, there are many questions regarding the 'new nursing standards' that are included in the order, as well as what the training and education requirements will look like for nurses."
The order is an emergency measure, and one that has taken significant time to implement. In the meantime, there is still a need for long-term investments in mental health and substance use care to build a system where providers feel supported and people get the care they need.
Picco believes that nurses are an important part of the solution. She says that with the right resources, they have the skills to help more people who are at risk from toxic substances. "They know their patients tremendously well, more so than the doctors often, and I think nurses are an excellent resource, and part of the solution to this problem."
But there is still a long way to go in expanding the supply of safe opioids and treatment options that are inclusive and culturally appropriate. (The rate of opioid poisoning deaths among First Nations people in BC is over four times higher than that of other residents.)
Following last year's order, trained nurses will first be able to prescribe Suboxone, and will later be trained on prescribing other alternatives like slow-release oral morphine and methadone.
Many harm reduction advocates argue that the new measures fall short of true safer supply, which would provide pharmaceutical-grade versions of illegal substances, such as diacetylmorphine, instead of alternatives.
Picco knows from experience how difficult it can be for substance users who cannot access a safe supply of diacetylmorphine. "Tommy went through methadone and suboxone, and despite several attempts with those, and even with rehab, it wasn't a solution for him."
She says that expanded treatment modalities are also critical.
"More attention needs to be paid to supporting mental health treatment. But at the same, the expectation of total abstinence is not an acceptable goal," she argues. "People who use alcohol are not automatically labelled alcoholics. And likewise, not everyone who uses illegal substances is an addict with a 'drug problem.' We just need to ensure that they can be safe in what they are doing,"
Federal Leadership Needed
Health-care delivery is a provincial responsibility, but the opioid crisis is national in scope, and provinces cannot adequately meet the challenge on their own.
Nationally, the number of preventable overdose deaths to date has far surpassed the total number of deaths of all other public health emergencies in the last 20 years including SARS, H1N1, Ebola and now COVID-19, yet the crisis has not achieved national emergency status.
"BC's nurses see the effects of the toxic drug supply public health emergency every day."
And still Ottawa has refused to declare the current opioid and fentanyl poisoning crisis a National Public Health Emergency under the Emergencies Act.
Such a move would unlock federal funding for evidence-based treatment programs such as the innovative program at Vancouver's Crosstown clinic that provides access to safe opioids like prescription heroin for those most at risk for overdose and poisoning.
"The federal government has an obligation to act because it has failed to control the illegal drug supply, or keep fentanyl out of it," Sorensen argues. "Over 80 percent of suspected opioid deaths last year involved fentanyl, and it was often combined with other drugs — most often heroin, cocaine or methamphetamine."
In the meantime, she says BCNU will continue the fight to reducing and eliminate preventable deaths and support the the thousands of family members like Picco who have been touched by the opioid crisis.
The pain of Picco's loss is still raw, but she takes solace knowing her son was able to make a difference in the lives of others after he died. "Tommy was able to donate his heart, his liver and two kidneys," she reports. "And as a nurse, that fact provides a bit of comfort." •
Bevel Up: Calling for Compassion, Anti-Stigma Education and Policy Change

Community nurses know that one of the biggest problems associated with the use of controlled substances is that those who use them are often reluctant to seek treatment due to the stigma they face. This exacerbates chronic health conditions, increases isolation and further adds to the complexities of the issue. The aversion often comes from the experience of being discriminated against by the very health-care workers who are tasked with providing care.
This reality was driven home in the 2007 film Bevel Up – Drugs, Users and Outreach Nursing. The stories told and lessons to be learned are still as current and relevant as ever in the wake of today's opioid crisis.
That's why BCNU is supporting the launch of a renewed outreach campaign for Bevel Up, an award-winning documentary and learning resource that has helped health-care workers deliver compassionate care to people who use drugs.
The initiative is a timely anti-stigma campaign that's pushing for policy change at all political levels. Producers hope to engage with many community partners and share of updated curriculum materials.
The film is and accompanying educational playlists are designed to give students and instructors in the health-care field access to the knowledge and experience of pioneering practitioners. In 2018, BCNU helped sponsor a relaunch of Bevel Up in a digital format to help raise awareness of the work nurses are doing in the midst of today's ongoing opioid crisis.
The camera follows street nurses as they reach out to people working in the sex trade, and people who use substances in the alleys and hotels of Vancouver's Downtown Eastside. Most importantly the nurses reflect on the attitudes they bring to their work—attitudes that can make or break their relationships with the people to whom they provide practical, non-judgmental health care on a daily basis.
The current opioid crisis, which has seen even more deaths than the COVID-19 pandemic in Canada, has meant that the film Bevel Up has even more relevance to communities. The launch of the new educational materials for Bevel Up will share important knowledge to nurse educators, point-of-care workers and communities dealing first hand with the opioid crisis. •
Watch the National Film Board documentary Bevel Up on your mobile device.
UPDATE (Spring 2021)
TAKING ACTION
NO END IN SIGHT AND MUCH MORE TO BE DONE
BC has been in a toxic drug public health emergency for five years. In that time, we will have lost almost 7,000 people to the toxic supply of opioids. Thousands of years of life and potential gone. We must turn this tide. Heath-care and policy leaders from all quarters – from the Coroners Service to the Association of Chiefs of Police to health-care providers and community advocates – agree that action must be taken in four broad areas:
1. PROVIDE ONGOING HARM REDUCTION MEASURES such as the widespread provision of naloxone, the expansion of overdose prevention sites, supervised consumption sites and drug checking services.
2. INCREASE ACCESS TO SAFE SUPPLY with prescribed pharmaceutical alternatives to reduce drug users’ reliance on a profit-driven illegal drug trade that depends on growing its customer base to increase its profits. Encouraging nurses and physicians to prescribe alternatives to their patients will save lives.
3. BUILD PROVINCIAL MENTAL HEALTH TREATMENT AND RECOVERY SERVICES that are regulated, evidence-based, economically and geographically accessible, and ensure this treatment is available when people are looking for it. Waiting weeks and months for access to recovery and treatment services means the difference between life and death.
4. END THE CRIMINALIZATION OF PEOPLE WHO USE DRUGS. We know that decades of stigma and punishment have brought us to the devastating place we are in today. We need to move from punishing and blaming to supporting and healing.