Sustaining Nursing in Canada
Sustaining Nursing in Canada

Solving Canada’s nursing shortage is a complex, multi-layered challenge. However, a new report from the Canadian Federation of Nurses Unions (CFNU) outlines a long list of solutions to the problem – and many of them aren’t complicated.
The 68-page document, Sustaining Nursing in Canada is a deep dive into the challenges that currently exist, from chronic staff shortages to the high prevalence of burnout in the nursing profession.
CFNU co-published the report with the Canadian Health Workforce Network. Authored by Dr. Houssem Eddine Ben Ahmed and Dr. Ivy Lynn Bourgeault, both from the University of Ottawa, the document presents a series of evidence-informed made-in-Canada solutions for tackling the seemingly intractable nature of Canada’s nurse shortage.
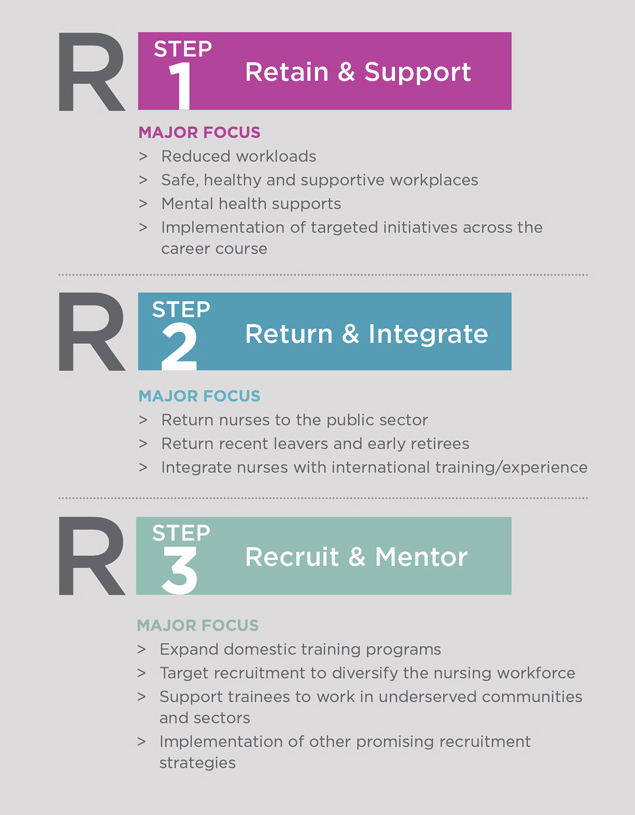
The report identifies “three Rs” that the authors say must be addressed to effectively tackle the nurse shortage in this country.
The first is the need to retain the existing workforce by reducing workloads, creating safe, healthy workplaces, providing mental health support and implementing targeted initiatives across the career-course.
The second involves encouraging nurses who have left the workforce, such as early retirees, to return. The third is the need to focus on recruiting and mentoring the nurses of tomorrow and diversifying the workforce so that all nurses feel included and represented.
In short, retaining experienced nurses to ensure the highest quality of care, returning nurses who have left to bolster an ailing workforce and recruiting and training the nurses of tomorrow to meet future needs.
BCNU president Aman Grewal says it’s time that policy makers listened more closely to nurses when considering both short- and long-term solutions to the problem.
“When we sit down with government and engage with decision makers, we make sure they understand that we are ready to help fix this crisis. Why not ask the people who are living and working this reality what solutions they’d like to see?
“Decision makers need to heed this report and apply some of its many proposed solutions.”
-BCNU President Aman Grewal
“This report includes many strategies that would make a difference if applied tomorrow,” she adds.
The arrival of the COVID-19 pandemic dramatically highlighted the serious shortcomings of BC’s health-care system, including a chronic nursing shortage which has led to increasingly difficult working conditions for nurses struggling to provide safe patient care during the public health emergency.
Grewal says nurses have been ringing alarm bells for years to warn that a nurse shortage was coming. But those warnings have been largely ignored, leaving nurses and other health-care workers with the current reality on the ground.
“The staffing shortage has reached such dire levels that we’ve seen temporary closures of emergency rooms in communities around BC,” she says. “This is happening so often that it’s become common to hear of people having to drive long distances to access care.”
She reports that nurses are experiencing unheard-of levels of moral distress from witnessing the ongoing and negative impact on patient care.
The latest workforce numbers from Stats Can show there are currently 5,325 nurse vacancies in BC, and by 2031, nearly 27,000 nurses will be needed to keep up with the health-care needs of an expanding population. BC is not alone. The situation is just as dire across the country as provinces and territories grapple with a shrinking workforce.
So how did we get to this point?
Sustaining Nursing in Canada details governments’ poor planning and failure to adequately address the systemic challenges of today’s crisis, and its impact on patients, staff and the entire health-care system.
Many of the strategies first implemented in the early 2000s to address the nurse shortage were time-limited and ad hoc. Ultimately, they failed to address the multi-layered reasons behind the slowly dwindling nurse workforce.
“What we are seeing today is a knee-jerk reaction to a problem that’s been brewing for years,” says Grewal, in reference to the recent announcement of renewed health-care funding from Ottawa to the provinces. “The new normal for a working nurse is a 16- to 18-hour shift without a break and no support, and that’s leading to high levels of burnout and exhaustion. We can’t continue expecting nurses to work in these conditions.”
The report also recommends the collection and effective use of data to provide a roadmap to avoid recurring and drastic nurse shortages, something the federal government also indicated was a priority during recent talks with the provinces that preceded the announced increase to the Canada Health Transfer. Sustaining Nursing in Canada’s proposed solutions to retain, return and recruit nurses could have a real impact on solving nursing shortages over time, Grewal argues, pointing to the report’s call for the adoption of a coordinated, evidence-based approach, which won’t just solve the crisis now, but head off future crises. “We are seeing the devastating impacts on working nurses now who are burning out as they try to carry the system on their backs,” says Grewal. “Decision makers need to heed this report and begin to apply some of its many proposed solutions.”
One of the report’s most timely recommendations involves internationally educated nurses already living in Canada but who have struggled with a complex, expensive and time-consuming registration process. It’s a situation that’s led to thousands of these skilled workers giving up their dreams of practising in this country.
Following years of BCNU advocacy, the provincial government announced in January that it would be making the changes necessary to help fast-track thousands of IENs into a system in desperate need of staff. BCNU welcomed the announcement and is cautiously optimistic the government will meet its own goal of creating 2,000 new positions in the next few months.
Sustaining Nursing in Canada highlights the positive impact that more accredited IENs will have on the system, but the report also outlines critical ideas and solutions that start at the work-site level, like creating peer and mentorship programs, supporting nurse leadership training, flexible scheduling, better wages and benefits and the creation of a public agency for mobile nurses.
Grewal wants the province to take heed of the wisdom contained in the report.
“Simply reading this report tells us that it’s not a matter of lacking solutions and ideas, but of implementing them,” she says. “Nurses have the solutions. We just need to be invited to the table.” •
THE THREE CRITICAL Rs OF NURSE WORKFORCE SUSTAINABILITY
How do we address the nurse staffing crisis now and support nurses in the future? We are going to need a series of evidence-informed made-in-Canada solutions to this complex, multi-layered problem. It starts with retaining our experienced nurses to ensure the highest quality of care; returning nurses who have left to bolster our ailing workforce; and recruiting and training the nurses of tomorrow to prepare us to meet future needs.
These are the recommendation contained in the latest report from the Canadian Health Workforce Network and the Canadian Federation of Nurses Unions.
UPDATE (Spring 2023)
EVIDENCE-BASED SOLUTIONS
The report Sustaining Nursing in Canada proposes a set of concrete actionable solutions to help meaningfully solve the health care staffing crisis. Published by the Canadian Federation of Nurses Unions and the Canadian Health Workforce Network, it highlights the magnitude of the nursing crisis and offers a path forward, so that patients can finally receive the care they need, and nurses can practice their profession under safe and sustainable working conditions.