Nurse-to-Patient Ratios Are Coming To BC
Nurse-to-Patient Ratios Are Coming To BC

It was a long time coming – and now that it’s here, it’s just the beginning. The government announcement on March 1 outlining the province’s commitment to implement minimum nurse-to-patient ratios in six distinct hospital-based care settings across BC was the culmination of an effort that started years earlier, when nurses began advocating for an effective policy solution to address their ongoing frustration with the way health care is staffed and managed in the province.
At the same time, health minister Adrian Dix’s announcement was but an early step on a new path and in a new policy direction whose ultimate course has yet to be charted.
The event followed months of work and consultation between BCNU, the Ministry of Health and health employers. Since the fall of 2023, working groups comprised of union leaders and staff, the health ministry and the Health Employers’ Association of BC have been meeting regularly to prepare for the planning and implementation of minimum nurse-to-patient ratios.
This ongoing effort includes establishing frameworks for monitoring and evaluating the impact of ratios, and developing polices for effective nurse retention, return and recruitment that will be crucial to the success of the effort.
The executive steering committee overseeing all of this work operates by consensus, and the announcement followed an agreement on the part of BCNU, the government and employers that BC will have a minimum staffing standard of one nurse for every four patients in medical/surgical units 24 hours per day, seven days per week, making our province the first jurisdiction in the world to establish such a standard (see table in sidebar).
BCNU President Adriane Gear joined Dix for the announcement and spoke to reporters about the importance of ratios for her members.
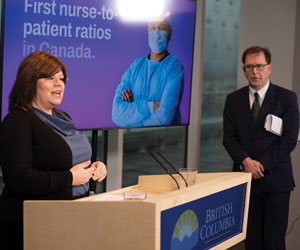
“We believe minimum nurse-to-patient ratios are the single most important policy solution available to address the staffing crisis that is gripping our health-care system,” she said, noting that ratios have been proven to improve job satisfaction, promote safe, healthy and supportive workplaces and generally improve the practice conditions needed to attract a new generation of nurses the province desperately needs.
“Today’s announcement also provides hope for nurses who are working in the health-care system now,” she added.
“We have a nurse staffing crisis and our focus must be on creating a robust nursing workforce,” she stressed. “We believe the framework in today’s announcement, along with a strong and competitive collective agreement, should go a long way to attracting those nurses who have left the health-care system to come back to the bedside.”
Attracting those nurses should be made easier with the $237 million in one-time funding initiatives that Dix announced to help retain, return and recruit new nurses into the health-care system to support the implementation of ratios. This includes $169.5 million for the expansion of provincial rural retention incentives and $69.5 million for training and licensing investments.
“Ratios are a strong, simple, clear mechanism that transparently indicates nurse staffing expectations across the province.”
- BCNU interim CEO Jim Gould
Patients and families are the ultimate beneficiaries, said Gear.
“It’s important to recognize that nurse-to-patient ratios will improve patient care by allowing nurses to devote time and attention to patients’ needs. The evidence shows that ratios save lives because they reduce patient mortality and incidents of missed care,” she noted.
“The promise of safer patient care makes us excited to get to work and puts BC on the map as the first province in Canada, and one of the first jurisdictions in the world to make ratios a reality,” she said.
The specific ratios announced at the news conference cover the majority of the acute care sector, but Dix also reiterated the government’s commitment to minimum nurse-to-patient ratios in long-term care and assisted living, and community and non-hospital care settings across the province.
Gear says the working groups are now focused on ensuring the successful implementation of minimum nurse-to-patient ratios in remaining hospital and non-hospital settings. An announcement for those sectors is scheduled for this June.
LAYING THE GROUNDWORK
The March 1 announcement may have signalled the beginning of the implementation process, but the starting point really began in April 2023, when the NBA, headed by lead negotiator and BCNU interim CEO Jim Gould, signed an agreement with the government committing the province to the adoption of minimum nurse-to-patient ratios.
This agreement established the initiative’s executive steering committee and governance structure and secured funding to begin implementation of ratios, including $200 million in 2023/2024, $250 million in 2024/2025 and $300 million in 2025/2026.

Gould says the time had come to push hard for ratios. Prior to the 2023 agreement, over 80 percent of BCNU members polled ahead of NBA bargaining said ratios were a top priority for improving working and practice conditions – the third highest after wage and staffing increases.
This is unsurprising. For over 25 years, BCNU has advocated for minimum nurse-to-patient ratios as an effective tool to address staffing and workload challenges. However, Gould notes that provincial governments had resisted the policy. Meanwhile, the existing tools negotiated to manage workload had broken down, resulting in lost trust.
“The workload assessment process in previous NBA contracts saw nurses face ongoing challenges reaching agreement with managers when attempting to align staffing levels with patient care needs,” he says, and notes the frustration members have reported when compelling employers to follow through with their staffing commitments.
Gould says he’s looking forward to nurses putting those days behind them.
“With ratios, we have a strong, simple, clear mechanism that transparently indicates nurse staffing expectations while providing a path forward to helping repair that trust.
“I’m very pleased the BC government has finally recognized the transformative potential of ratios and made a significant commitment to their funding and implementation across the province,” he adds.
BUILDING ON THE EVIDENCE
Gould’s optimism is inspired by the success of minimum nurse-to-patient ratios in other health-care systems.
“We have a unique opportunity in BC to learn from the experience of nurses and employers in California and Australia, and tailor our approach to achieve the successes seen in those jurisdictions,” he says.
In Sacramento, nursing vacancies decreased by 69 percent within four years of the implementation of ratios. And hospitals across California saw turnover and vacancy rates fall below five percent, well below the national average. Meanwhile, in Victoria, Australia, the number of employed nurses grew by more than 24 percent, with over 7,000 inactive nurses returning to the workforce after the implementation of minimum nurse-patient ratios in that state.
“We have a unique opportunity in BC to learn from the experience of nurses in other jurisdictions.”
- BCNU interim CEO Jim Gould
Numbers like these tell Gould that the sooner BC’s health-care system can be stabilized with nurse staffing ratios the sooner the province can end the use of costly and destructive nursing agencies.
The exodus of nurses from the public health-care system following the COVID-19 pandemic has seen health authorities turn increasingly to these expensive for-profit staffing businesses, spending tens of millions of dollars in an attempt to staff unfilled positions. But the grueling and unsustainable working conditions mean many nurses have no interest or ability to return, and the more than 5,000 nurse vacancies in the province are making it increasingly difficult to meet people’s health-care needs.
The Ministry of Health put a moratorium on onboarding new agency contracts in November 2022, but existing contracts remain.
“The over-use of agency nurses is destroying the team-based culture necessary in the long-term to support a healthy work environment and optimal patient outcomes,” says Gould, who notes that health authorities are spending millions of dollars on for-profit agencies to bring nurses to the bedside and fill the staffing gap.
BC agency nursing hours saw a four-fold increase between 2019 and 2023, with over 1.1 million hours worked by agency nurses in the 2022/23 fiscal year. Gould says it’s an expensive and unsustainable health human resources strategy that’s grown from at least $8.7 to $64 million since the pandemic began.
CONTINUING THE WORK
Gear says she’s keen to observe how minimum nurse-to-patient ratios will improve patient care by helping retain the nurses we have now, return nurses back to the bedside and recruit new nurses. But the promise of ratios depends on her efforts and that of Gould and a host of BCNU elected leaders and staff who have been working on a daily basis for months to tackle the details of policy planning and implementation.
“Almost all of the work of the executive steering committee and working groups involves detailed analyses and negotiations before all parties reach consensus,” she explains “Operational considerations, such as unit and bed gap analyses, reporting and monitoring methodologies, retention and recruitment strategies and approaches to change and risk management are all part of the nurse-to-patient ratio implementation planning template we are creating with health employers.”
“Direct care nurses’ involvement will be critical for the planning and implementation of ratios in BC.”
- BCNU President Adriane Gear
BCNU members and staff on this project are also working to finalize the Ministry of Health’s policy directive that spells out specific employer obligations on a range of policies related to staffing ratios. Much of this work has involved developing and reaching consensus on such things as the definition of med./surg. – where the majority of acute care nurses work – and the definition of chronic overcapacity for the purposes of creating rotations that are able to achieve the 1:4 ratio. It has also involved discussion on how and what kinds of relief to include in the ratio and the use of absolute vs. average numbers of nurses when determining if a unit is in ratio.
A SHARED JOURNEY
Gear says direct care nurses’ involvement will be critical for the planning and implementation of ratios in BC, and the effort’s success will depend on BCNU members’ participation in monitoring and evaluating nurse-patient ratios at worksites across the province.
“The work has just begun,” she says. “It’s important that nurses have their voices heard. That’s why we’re consulting with members through surveys and focus groups and seeking nurses’ participation in monitoring and evaluating mNPRs at worksites across the province.”
Gear encourages all members to visit the BCNU website and submit an expression of interest to participate in the monitoring and evaluation process at their worksite.
“Let’s do this together and make nurse-patient ratios a reality!” •
UPDATE (Spring 2024)
MINIMUM NURSE-TO-PATIENT RATIOS ARE BEING ESTABLISHED IN THE FOLLOWING ACUTE HOSPITAL CARE AREA SETTINGS:
| SETTING | RATIO |
| General Medical/Surgical Inpatient (Adult/ED/Pediatric) |
1:4 24/7 |
| Rehabilitation | 1:5 Day/Evening 1:7 Night |
| Palliative | 1:3 24/7 |
| Focused (Special) Care (Adult/Child) | 1:3 24/7 |
| High Acuity/Step Down (Adult/Child) | 1:2 24/7 |
FIRST STEP Minimum nurse-to-patient ratios are being established in the majority of care areas within acute hospital settings. This puts BC on the path to become the first jurisdiction in the world to have a minimum staffing standard of one nurse for every four patients in medical/surgical units 24 hours per day, seven days per week. Implementation planning in health authorities began in March 2024 and nurses working on med./surg. units will begin to see changes in staffing allocations to reflect the 1:4 minimum nurse-to-patient ratio by fall 2024.
MEMBERS’ VIEW
The work is now underway to make BC the first province in Canada to implement minimum nurse-to-patient ratios in health care settings. We asked a group of BCNU South Fraser Valley region members about their hopes for nurse-to-patient ratios in addressing the staffing challenges nurses face.
BRYANT GANADIN
Surrey Memorial Hospital
"My hope is that nurse-to-patient ratios will work. I work on a medicine unit and I feel that medicine is such a huge bulk of the patient population in many of the hospitals but there is less focus on it. There is a lot of turnover in medicine despite the hiring efforts. It’s hard to retain people these days and I think it’s because of the high workload. I’m hoping that, with ratios, we can hold the employer accountable and find a way to provide excellent care with the right amount of patients for each nurse."
LYANNE LAMANILAO
Langley Memorial Hospital
"One of my hopes for nurse-to-patient ratios – especially for RNs – is that they address not just the number of patients we handle, but also the acuity level. We are dealing with patients who are more acute since COVID and patients’ issues are more complex. I also hope ratios mean more students and younger nurses will stay in the profession to help sustain the health-care system."
COURTNEY GLOUX
Surrey Memorial Hospital
"Better ratios means better care! And safer care, too. My hope is that the implementation of minimum nurse-to-patient ratios means families can get all-encompassing aspects of physical, emotional and spiritual support from me. It also means less risk of caregiver burnout and fewer mental health challenges for nurses to manage."